Focal Knee Resurfacing Implant: A Much-(K)needed Treatment for Middle-aged Patients!
Maastricht University (NL)
Amin Abrishamkar
“New treatment on the horizon for bridging the treatment gap for middle-aged patients on the verge of osteoarthritis.”
Sounds like medical jargon gone wild, doesn't it? Fear not – this blog aims to unravel the story behind this groundbreaking piece of medical news.
Tiny Tears, Big Trouble
Injury to articular cartilage is widespread and associated with pain and swelling, with knee being the most frequently affected joint. Due to the avascular and aneural nature of articular cartilage, i.e. no blood and no nerve supply, it has very limited inherent healing potential, meaning that damage to cartilage will most likely lead to a permanent defect.
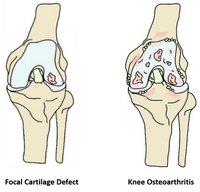
Focal cartilage defects (FCD) are common knee injuries, often caused by trauma. FCDs are localized areas on the articular surface where the cartilage is completely or partly torn away (Figure 1). Symptomatic FCDs can impair patient’s quality of life to the same extent as severe osteoarthritis (OA), and if left untreated, may progress to OA in the long term [1].
Joint Preservation: Putting the Brakes on Knee Replacement
Orthopedic surgeons employ a variety of strategies, ranging from biological and regenerative-based approaches to joint replacement, to alleviate symptoms and restore function caused by FCD. While biological cartilage repair techniques, such as Microfracture (MF) and Autologous Chondrocyte Implantation (ACI), have shown high efficacy in younger individuals, patients over the age of 40 may experience inferior clinical outcomes and recurring symptoms due to age-related decline in regenerative capacity [2]. What all cartilage repair techniques have in common is the ultimate goal of joint preserving in middle age by postponing or eliminating the need for joint replacement.
Figure 1. Focal cartilage defect and osteoarthritis in the knee joint
Younger isn’t always better!
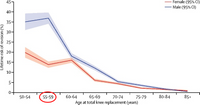
Joint replacement (aka Arthroplasty) constitutes the mainstay of surgical intervention on the extreme end of the treatment spectrum and is considered as the “gold standard” surgical treatment for end-stage OA. Despite high survival rate of arthroplasty in aged patients, studies have demonstrated a dramatic increase in the lifetime risk of revision surgery for patients below the age of 60 [3] (Figure 2). A revision surgery is performed when a patient who has had a primary knee replacement experiences unsatisfactory results or complications, requiring a follow-up procedure. Such re-operations are associated with unfavorable outcomes and high complication rates, leading to substantial morbidity and increased healthcare costs [4].
Age is just a number. But is it?!
Now let’s take a moment to ponder where the issue arises. Did you notice the age limits in the last two paragraphs? That’s right, there is a gap for patients between the age of 40 and 60, commonly referred to as middle aged. Patients in this age group pose a challenge to orthopedic surgeons, as they may be too old for regenerative-based treatments, yet too young for arthroplasty. According to a survey [5], 4 out of 5 orthopedic surgeons perceive “a need for better treatments for middle-aged, physically active early OA patients in which Figure 2. Lifetime risk of revision after total knee replacement [3] arthroplasty is not indicated”. It becomes even more striking when we realize that around 60% of all cartilage surgeries are performed on middle-aged patients. This highlights a glaring treatment gap for the very demographic most in need of care! But how to address the gap? The short answer is Focal Knee Resurfacing Implants.
Filling the Treatment Gap
A focal knee resurfacing implant, or FKRI, is a partial resurfacing device for treating full-thickness cartilage defects. The implant has a cartilage-mimicking cap that fills the defect site and is anchored to the subchondral bone via a solid stem (see Figure 3). This mini-implant is introduced via a minor invasive surgery, allowing for a fast rehabilitation and a swift return to work. During this resurfacing procedure, minimal amount of tissue is removed or replaced, thus preserving the native anatomy of the joint for potential joint replacement in case of implant failure later in life [6], hopefully not before the age of 60. Thanks to its joint-preserving aspect, FKRI can potentially serve as the primary surgical intervention before considering arthroplasty for middle-aged individuals with full-thickness cartilage defects or those with failed biological treatments.
SyCap: Pioneering the Future of Knee Resurfacing Implants
Synthetic Cartilage Plug, or SyCap, is a focal knee resurfacing implant currently being developed by Avalanche Medical (Maastricht, the Netherlands). SyCap is a non-degradable implant made of polycarbonate urethane (PCU) with mechanical and tribological properties approximating human tissue, ensuring wear resistance, long-lasting functional restoration and pain relief, without inducing damage to the opposing cartilage. The polymer implant is radiopaque (visible on X-ray) and is fully magnetic resonance imaging (MRI)-compatible, thereby allowing for unrestricted post-operation monitoring. In the event that revision or conversion becomes necessary, SyCap can be readily converted to a larger implant or even knee arthroplasty.
Figure 3. Focal knee resurfacing implant for the treatment of focal cartilage defects
[Source: Avalanche Medical]
From Bench to Bedside
Our team at OSTASKILLS is dedicated to advancing medical devices in the management of osteoarthritis, with a particular focus on bridging the treatment gap for middle-aged patients suffering from cartilage defects in the knee joint. Through rigorous preclinical studies and first-in-man trials, we strive to ensure the efficacy and safety of this innovative solution, aimed at addressing the existing need for a better treatment for the target patient population.